AI Automation in Insurance Claims Processing

Don’t miss what’s next in AI.
Subscribe for product updates, experiments, & success stories from the Nurix team.
Artificial Intelligence (AI) has emerged as the powerful solution to the labor and time-intensive process of claims processing in insurance. By automating various aspects of the claims journey, from initial data gathering to final decision-making, resulting in significant time and cost savings.
A key advantage of the AI claims process is the ability to rapidly analyze claim documents, photographs, and other supporting evidence, identifying relevant information and detecting potential fraud with remarkable precision. This streamlines the initial assessment phase, allowing claims representatives to focus on complex cases that require human intervention.
The integration of AI into the insurance claims process also leads to more accurate and timely claim settlements, as well as enhanced customer experience for policyholders.
Next, let’s take a deeper look at how AI claims processes are already revolutionizing insurance.
The AI-Driven Revolution In Claims Management
According to the latest Gallagher Bassett report, 42% of insurers worldwide have already incorporated AI into their claims management processes, with a further 44% having started work on AI integration.
This widespread adoption of AI insurance platforms can be attributed to automation of routine tasks, enhancing decision-making, and speed and precision. These platforms can also help insurers analyze data in real-time, identify patterns, and make informed decisions quickly. This reduces processing time and errors, leading to increased efficiency, improved accuracy, and better customer satisfaction.
But to leverage the benefits of AI in claims management, you first need to understand the key capabilities it unlocks.
Key Capabilities Of AI In Claims Automation
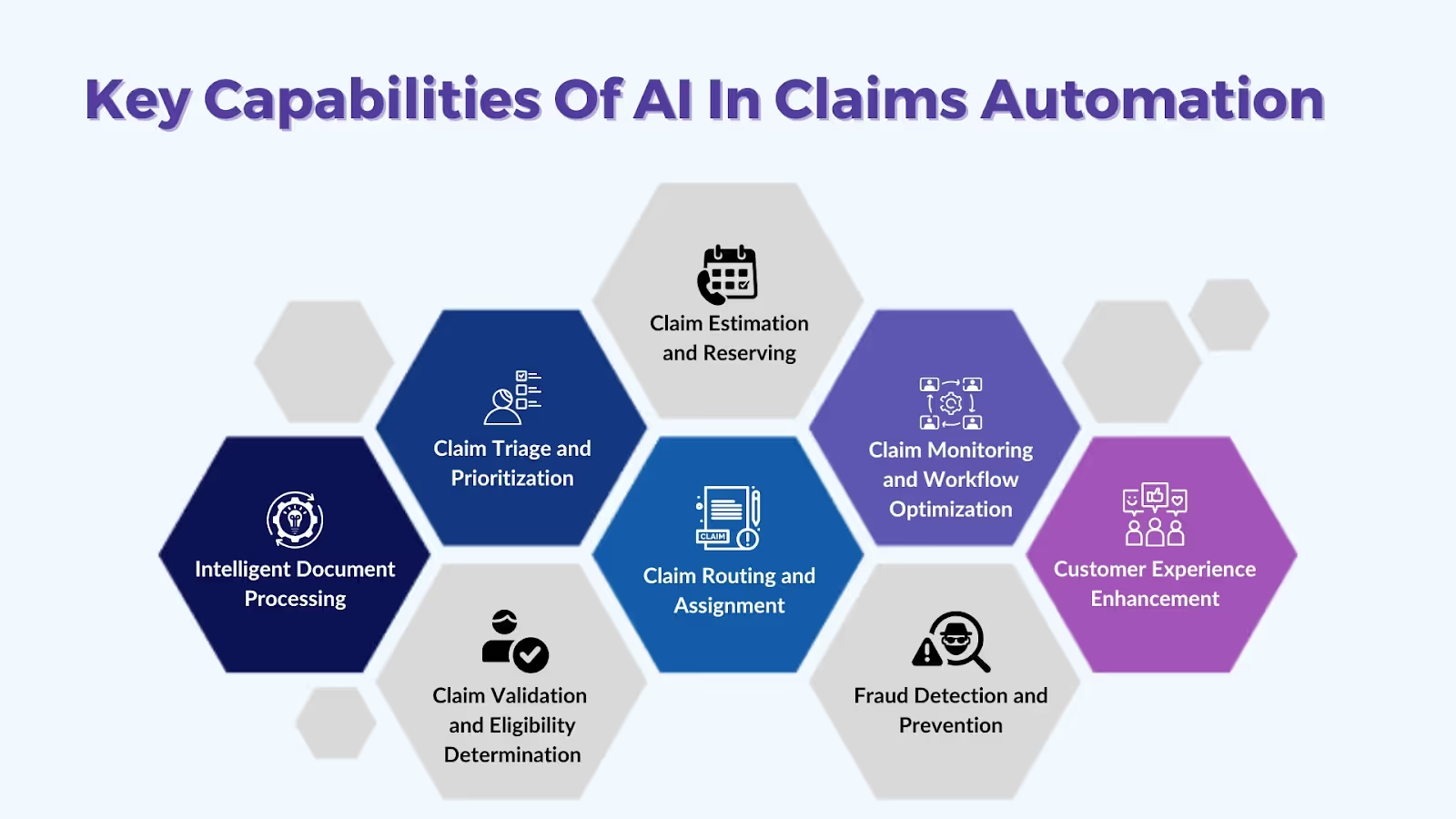
Here are some of the key capabilities of AI that can be beneficial to the claims automation process:
- Intelligent Document Processing: AI can automatically extract relevant data from claims documents, such as policy details, loss descriptions, and supporting evidence.
- Claim Triage and Prioritization: AI systems can classify claims based on complexity, severity, or risk, and prioritize high-value or time-sensitive claims for faster processing.
- Claim Validation and Eligibility Determination: AI insurance platforms are capable of automatically verifying policyholder eligibility and coverage details, and validate claim details against policy terms and conditions.
- Claim Estimation and Reserving: AI-powered predictive modeling can estimate the cost and duration of claim resolution, determine appropriate claim reserves based on historical data and industry benchmarks, and identify potential outliers or high-cost claims for further review.
- Claim Routing and Assignment: AI systems can route claims to the appropriate adjusters or specialists based on expertise, workload, or geographic proximity, which results in efficient processing.
- Claim Monitoring and Workflow Optimization: Insurance companies can use AI to track and monitor claim status and progress in real-time. This helps in identifying bottlenecks or delays in the claims process for process improvement.
- Fraud Detection and Prevention: Machine learning algorithms used by AI systems can identify patterns and anomalies indicative of potential fraud. By leveraging them, insurance companies can proactively assess risks and develop mitigation strategies to minimize fraudulent claims.
- Customer Experience Enhancement: AI platforms provide self-service capabilities for policyholders, automated communication and updates, and personalized claim handling and recommendations based on customer preferences and historical data.
Insurance companies can leverage these AI capabilities to streamline the claims process, improve operational efficiency, enhance customer experience, and reduce the overall cost of claims management.
The most prominent benefit of using an AI claims management system is the enhanced operational efficiency. Let’s dive into some use cases of the same.
Enhancing Efficiency with AI Claims Automation
AI-powered claims automation can streamline workflows from submission to settlement. This accelerates resolution and ensures consistency in decision-making. Here are a few use cases of AI enhancing efficiency:
Streamlining Claim Status Checks And Bill Edits For Faster Resolution
AI claims processing can leverage machine learning algorithms to automate tedious claims tasks, reducing errors and improving accuracy. AI systems can quickly access patient records, provider contracts, and guidelines to identify issues and facilitate prompt resolution.
AI claims systems can also learn from past data to predict and preempt problems, minimizing back-and-forth between providers and insurers. This accelerates the overall claims resolution timeline, benefiting patients and providers.
Simplifying The Prior Authorization Process To Reduce Delays
By automating documentation review and analysis, AI can expedite the approval process. This saves time, minimizes errors, and provides real-time feedback to healthcare providers. As a result, patients can receive care more promptly, improving outcomes, and enhancing the experience for both providers and individuals.
Efficient Management Of Denials To Minimize Revenue Losses
AI's ability to analyze data and identify denial patterns allows insurance providers to proactively address common issues like coding errors. Real-time alerts and recommendations from AI-driven claims processing can help organizations address denials promptly, preventing accumulation and financial setbacks.
AI can also automate the appeals process, freeing up staff to focus on complex claims management, thus, reducing administrative burdens and optimizing revenue management.
In addition to enhancing operational efficiency, AI claims management can also improve accuracy and preemptively prevent fraud.
Role Of AI Claims Management In Boosting Accuracy And Preventing Fraud
AI claims management systems use analytics and machine learning to boost processing accuracy and identify fraudulent claims. Here are a few use cases of the same:
Role Of AI In Enhancing Data Processing And Verification Accuracy
AI-powered systems can analyze claims data with speed and precision, allowing insurers to streamline the claims process. These systems can identify patterns, anomalies, and inconsistencies that would be challenging for human reviewers to detect. This heightened scrutiny helps mitigate the risk of fraudulent claims, ensuring payouts are made only for legitimate cases.
AI's rapid data processing enables insurance companies to make more informed and timely decisions, improving the customer experience. Automating the claims review process and flagging issues for investigation allows faster turnaround and more responsive service, enhancing satisfaction and operational efficiency.
Leveraging Advanced Analytics For Effective Fraud Detection
Advanced analytics can effectively detect insurance fraud, yielding significant benefits for insurance providers. By analyzing claims data, AI systems can uncover patterns indicating fraudulent activity, enabling proactive mitigation of losses.
Sophisticated algorithms and predictive modeling identify high-risk profiles and suspicious behaviors that would be difficult to detect manually. This data-driven approach enhances fraud detection accuracy and allows companies to focus investigative efforts on high-risk claims.
Impact Of Predictive Analytics In Risk Assessment And Estimation
Predictive analytics enables AI claims systems to forecast claim likelihood and impact using data and algorithms. Insurance providers can leverage this to price policies competitively, allocate resources effectively, and provide tailored coverage.
Integrating predictive analytics into claims processing has enhanced fraud detection and mitigation, protecting the insurance system and keeping premiums affordable for honest customers.
AI-Based Damage Inspection And Assessment
AI can improve remote damage inspection and analytics-based damage assessment for faster and more efficient claims processing. It can leverage automated image analysis to identify and categorize damage types, and assess damage severity for quicker initial estimates and settlements. Not only does this eliminate human error for more objective evaluations; it also ensures standardized damage assessments, which leads to faster reimbursements, reduced operational costs for insurers, and improved customer satisfaction.
AI damage inspection and assessment can also enhance fraud detection. These systems leverage computer vision, machine learning, and natural language processing capabilities to identify suspicious patterns in images and claim history, and automatically flags suspicious claims for investigation.
AI-Powered Customer Experience and Support
Insurance companies can make frustrating and overwhelming claims experiences more seamless and pleasant by leveraging AI-powered chatbots. These chatbots can be programmed to guide customers through the claims process, answering common questions, collecting necessary information, and even initiating the claims submission.
This not only streamlines the experience for the customer but also frees up human agents to focus on more complex issues. With real-time access to customer data and claims information, these AI assistants can provide personalized support and updates throughout the process.
With such a significant boost to efficiency, accuracy, fraud prevention, and excellent customer experience, investing in AI-claims management solutions is a no-brainer.
However, as with any new technology, it comes with its own set of challenges, which we’ll examine next.
Challenges And Solutions In AI Adoption
Adopting AI in insurance claims processing requires navigating accuracy and data security challenges. Insurance companies must implement robust data protection measures to safeguard policyholders' information. They must also implement stringent data security protocols to prevent unauthorized access, breaches, and misuse of sensitive details.
In addition, insurance providers must ensure data accuracy for AI-driven claims processing to flawlessly evaluate complex scenarios and uphold the integrity of the insurance system.
This means ensuring a seamless integration of legacy systems with new AI capabilities. Here are some strategies for accomplishing this:
- Conduct a thorough assessment of your existing insurance systems, data, and workflows to identify areas where AI can be most impactful.
- Create a detailed roadmap for integrating AI into your insurance operations, considering both short-term and long-term goals.
- Identify the necessary data, infrastructure, and technology requirements to support AI implementation. And establish clear governance frameworks, data management protocols, and change management strategies.
- Ensure your data is clean, structured, and accessible to enable effective AI-driven decision-making to seamlessly integrate disparate data sources across your organization, including policy information, claims data, customer profiles, and external data.
- Identify tasks and processes that can be effectively automated, while maintaining human oversight and decision-making for more complex or sensitive matters. Then design workflows that seamlessly blend human expertise and AI-driven automation, leveraging the strengths of both.
- Provide comprehensive training and change management support to help employees adapt to the new AI-augmented workflows.
- Implement a modular and scalable AI platform that can integrate with your existing insurance systems and leverages cloud-based AI services and tools for scalability, flexibility, and easy deployment.
- Develop robust performance metrics and KPIs to track the impact and effectiveness of your AI-powered insurance solutions. Regularly review and refine your AI integration strategies based on feedback, user experience, and evolving business needs.
- Continuously optimize your AI models, workflows, and processes to drive ongoing improvements and maximize the benefits of AI integration.
By now, you may be thinking that all of this is beyond your expertise and knowledge. So how do you go about integrating AI systems into your claims processing and other operations?
The solution is Nurix AI. We customize solutions for customer interactions that adapt, evolve, and deliver tangible business value for you. Contact Nurix for your AI integration needs today.

Don’t miss what’s next in AI.
Subscribe for product updates, experiments, & success stories from the Nurix team.









